TABLE OF CONTENTS
Laminitis in Horses
Laminitis (Founder) in Horses is the inflammation of the sensitive laminae of the foot. It is common in fore-foot. Ordinarily one or two feet may be affected. Sometimes all the four feet are affected. The symptoms are produced by a derangement of the vasoconstrictor nerves, thereby causing a congestion of the laminae.
Laminitis in Horses is not a primary disease, but usually occurs as sequelae to 4 different clinical entities–
- Diseases associated with sepsis/endotoxemia
- Excessive weight placed on a limb due to injury to the opposite limb
- Cushing’s disease in the older horse
- Equine metabolic syndrome (EMS) including pasture-associated laminitis
Etiology
- Heavy body weight
- Flat, spreading feet
- Enterotoxaemia resulting from eating
- Excessive intake of grains like barley and wheat or high proteinaceous feed
- Drinking of cold water immediately after hard work
- Concussion, especially due to fast work on hard ground
- Overwork
- Toxemia resulting from pneumonia, metritis, retained placenta, etc.,
- Superpurgation
- Vasoconstriction
- Arteriovenous (AV) shunting in digital laminae
- Coagulopathy
The three main presentations of laminitis are-
- Those associated with bacterial sepsis
- Those associated with metabolic/endocrine disorders, and
- Those associated with excessive concussion/weight-bearing
The predisposing diseases associated with bacterial sepsis include retained placenta, surgical acute abdominal cases (usually involving severely compromised segments of the intestine), enterocolitis, pleuropneumonia with a Gramnegative component, and carbohydrate overload (which usually results in a severe transient enterocolitis).
Metabolic/endocrine disorders that predispose to laminitis are primarily associated with equine metabolic syndrome (EMS), also commonly termed “pasture-associated laminitis.” A low level of systemic inflammation has been reported to be present in horses with EMS (similar to that observed in human metabolic syndrome), which may lower their threshold to other insults associated with laminitis.
Finally, supporting limb laminitis is a devastating sequela to animals supporting an excessive amount of weight on one limb, usually due to an injury to (and commonly orthopaedic surgery on) the contralateral limb. Although little is known regarding the pathophysiology of this disease process, there is some evidence that decreased laminar blood flow may play a role in this type of laminar failure.
Clinical Signs
The clinical signs assessed in Laminitis in Horses mainly refer to the degree of lameness noted and the digital exam. The lameness varies in severity from being barely detectable to an animal that is recumbent the majority of the time due to the digital pain.
Due to this variability, more than 60 years ago Obel introduced a grading system to describe the degree of lameness. Although the Obel grading system does not describe all cases of laminitis, it is still used to describe the degree of lameness in both the clinics and when describing time points assessed in laminitis research.
Grade associated lameness and gait abnormalities
- At rest the horse alternately and incessantly lifts the feet, often at intervals of a few seconds. Lameness is not evident at the walk, but a short stilted gait is noted at the trot
- The horse moves willingly at a walk, but the gait is stilted. A foot can be lifted off the ground without difficulty.
- The horse moves very reluctantly, and vigorously resists attempts to have a foot lifted off the ground.
- The horse refuses to move and will not do so unless forced.
- Lameness
- Increase in temperature in one or more feet
- Increased digital pulse
- Elicitation of painful withdrawal response to hoof tester
- The characteristic stance of a laminitic horse with both forefeet affected is placement of the forefeet well in front of the normal position and anterior placement of the hind feet in order to shift more weight to the hindlimbs
- Stiff limb movement
Acute Laminitis
Clinical Signs
- Dull and has an anxious expression
- Elevated temperature (103 to 106˚F)
- Increased digital pressure
- Respiration accelerated
- Conjunctiva is injected
- Local symptoms of acute inflammation seen in the hoof
- Acute symptoms of laminitis usually subsidies within four to twelve days followed by recovery or progression into chronic laminitis. But very severe cases may terminate fatally.
In the severe case of acute laminitis there is intensification of the symptoms due to profuse exudation and haemorrhage into the sensitive laminae. Haemorrhage is due to rupture of distended vessels resulting from the pressure of body weight conveyed through the ospedis. The collection of blood or exudates causes severe pain and the animal lies, sweating profusely. It may groan with pain. Occasionally the blood or exudates may escape through the coronet region. This may be followed by gangrene because of infection gaining entrance into the inflamed tissue. The onset of gangrene may show a temporary relief from pain and give a false hope of recovery. But cases in which gangrene has set in are usually fatal.
Diagnosis
- From clinical signs and symptoms
- PD nerve block
- Radiograph – Lateral and dorsoplantar/palmer view
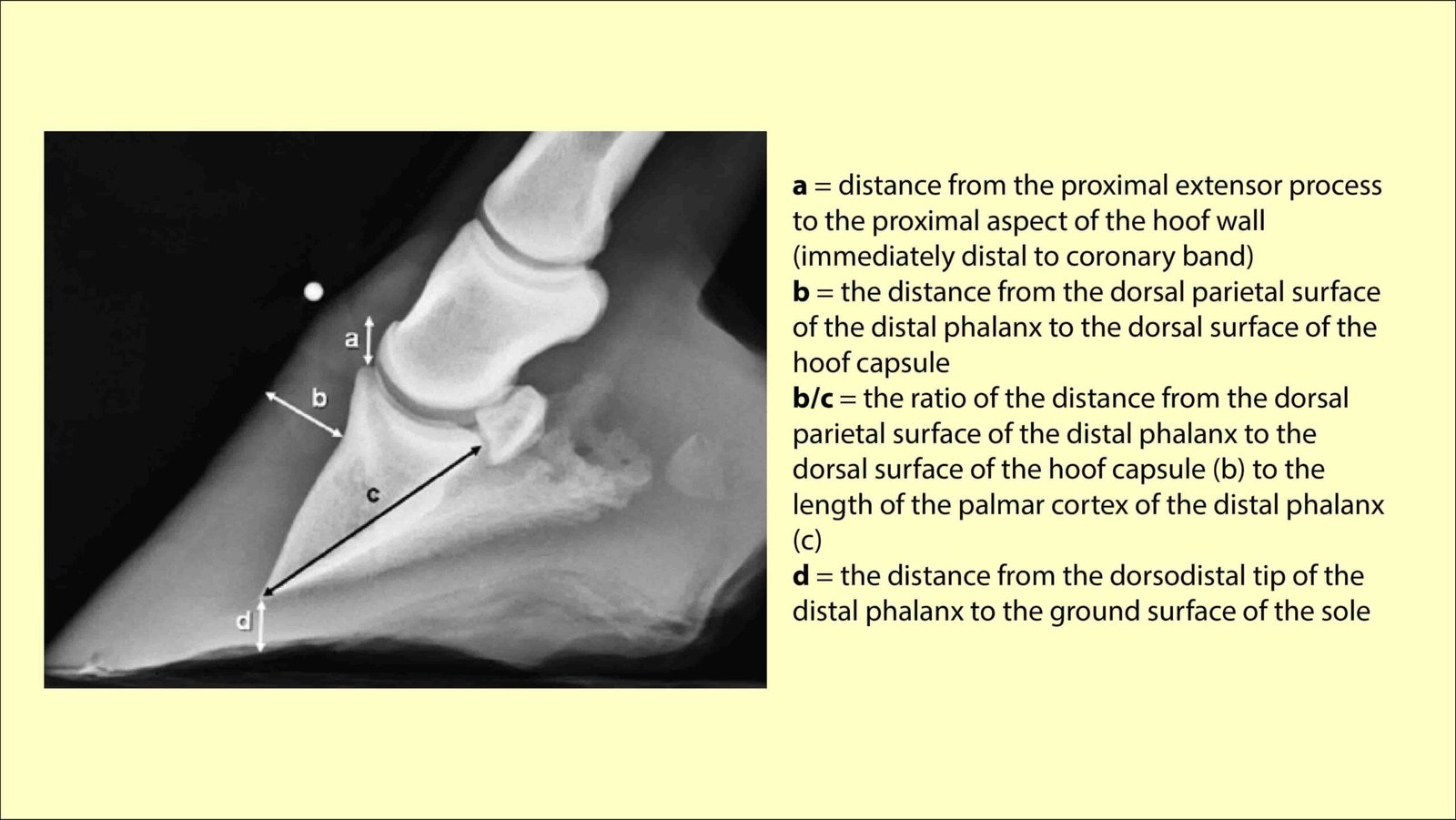
Early radiographic signs suggestive of distal displacement of the distal phalanx include widening of the distance between the dorsal hoof wall and the parietal surface of the distal phalanx, and increased vertical distance from the proximal aspect of the extensor process to the firm proximal border of the hoof wall located immediately distal to coronary band (sometimes termed the founder surface of the hoof capsule).
Prognosis
Depends on the severity of the attack. Prognosis is usually favourable when one limb is affected. When all the four feet are affected, it is guarded.
Treatment
- Cold application
- Inducing purgation (except in cases where laminitis is due to superpurgation, metritis and pneumonia).
- Anti-histaminic drugs
- Corticosteroid administration- Hydrocortisone 100 to 600mg diluted in 500 to 1000 ml of 10% Dextrose or isotonic Normal saline intravenously
- Fluid therapy to counteract toxaemia.
- Put the animal in laxative diet containing bran, linseed, green grass etc., magnesium sulphate and potassium nitrate may be added to the drinking water for laxative and diuretic effect
- PD nerve block
- Jugular phlebotomy may be done to reduce the blood volume and thereby to relieve congestion in the senisitive laminae. About 1 to 2 gallons of blood can be removed from a horse
- Auto-haemotherapy: Frank has reported this to be beneficial in the early stages of laminitis. 80 to 120 ml of blood is drawn out of the jugular vein and injected in to the same animal intramuscularly.
Chronic Laminitis
Clinical Signs
The foot changes in shape as a result of chronic laminitis. The changes are caused by the rotation of os-pedis on its horizontal axis.
The anterior portion of the soul becomes flat or convex. This is called dropped sole. The sensitive laminae of the sole undergo pressure atrophy and fails to secrete new horn due to compression of os-pedis. So when the horn of the sole wears off there may be perforation of the sole anterior to the frog. This exposes the sensitive tissues to infection and necrosis and consequently a serous or purulent discharge may be noticed.
Excessive growth of toe region and foot is elongated antero-posteriorly
The rings or rugae on the wall representing horn growth became more prominent because of the increased secretion of horn.
The white line of the foot became more prominent and thick due to separation of wall and the sensitive laminae and deposition of abnormal horn between them.
As the horse put more weight on the heels during progression, the toe is pushed forwards and upwards and as a result of this the lower portion of the anterior aspect of the hoof approaches a horizontal direction.
Treatment
- Remove all the excess horn
- Therapeutic shoeing
- A strip of leather or thin metal plate may be placed between the shoe and foot, so as to prevent the sole touching the ground
- If the sole is perforated, antiseptic foot bath (10% formalin) and antiseptic dressing (triple sulphate dressing) are recommended.