TABLE OF CONTENTS
Hormonal Regulation of arterial pressure
Hormonal Regulation of arterial pressure is maintained by sympathetic system and Renin-angiotensin system.
The sympathetic system influences the cardiovascular system through the release of neurotransmitter norepinephrine (NE) and also activates adrenal medulla to release epinephrine (EPN).
The EPN and NE activate membrane receptors called adrenergic receptors on the cardiac muscle cells and on the endothelial or smooth muscle cells of blood vessels.
The adrenergic receptors include α and β receptors which are subdivided into α1 & α2 and β1 & β2. The EPN and NE act through α receptors and causes arteriolar vasoconstriction. Resistance to blood flow is increased and total peripheral resistance (TPR) increases.
These hormones also produce venoconstriction (α receptor activation), blood is displaced to central circulation and ventricular preload increases. The hormones also activate β receptors in heart and increases rate and force of cardiac contraction resulting in increased stroke volume, TPR, preload and resulting in elevation of BP.
EPN has an affinity for both α and β receptors causes increased cardiac output, decreased peripheral resistance in skeletal muscle (vasodilatation) and elevated BP, whereas the NE has high affinity for α receptors but low affinity for β receptors causes vasoconstriction and rise in BP.
Renin-angiotensin system
Renin-angiotensin system start when there is decrease in renal arterial pressure, ECF or blood volume, stimulation of sympathetic nerves or disturbance in ECF sodium level causes release of renin from the juxta glomerular apparatus of the kidneys.
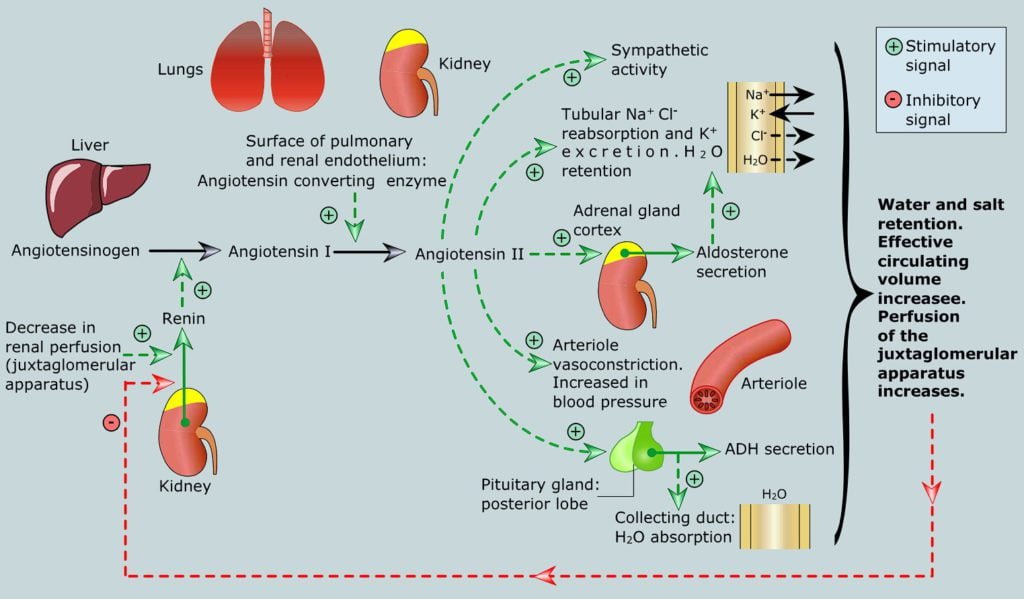
The renin, a proteolytic enzyme, splits angiotensinogen, a plasma α2 globulin (synthesised from the liver) to form angiotensin-Iby the enzymatic action in the kidney.
Angiotensin–I is converted to angiotensin-IIby the enzyme system present in the capillary endothelium of lungs. The angiotensin-II is a very powerful vasoconstrictor and destroyed by angiotensinases in peripheral capillaries.
Angiotensin-II stimulates aldosterone release from adrenal cortex. Aldosterone acts on the thirst centre of the hypothalamus, and renal tubule causes increased water intake and retention of sodium and water from the renal filtrate.
Aldosterone also causes vasoconstriction. All the three actions of aldosterone elevate the BP to normal.
Vasopressin
Vasopressin physiological role is related to long term regulation of Blood pressure brought about by water reabsorption from the kidneys.
In hemorrhage, large amounts of ADH are released to bring about vasoconstriction. When the BP undergoes change, after few hours to few days the nerves loose their power to control pressure because receptors adapt. Long-term mechanisms come into play, which involve renal fluid volume-pressure control mechanisms.