TABLE OF CONTENTS
Angiotensins
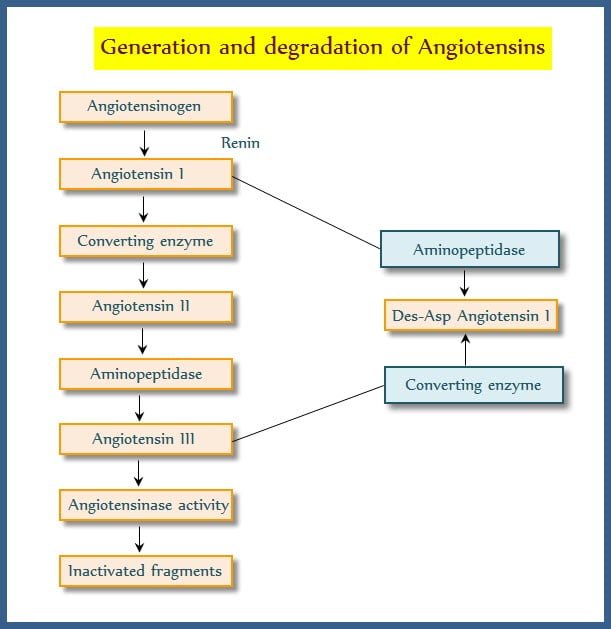
Angiotensins II is a octapeptide generated in the plasma from plasma alpha globulin involved in electrolyte, blood volume and pressure homeostasis. Enzyme renin is responsible for the pressor effects, later it became evident that the angiotensin converting enzyme (ACE) which is responsible for the formation of inactive fragments of Angiotensin I to Angiotensin II (potent vasoconstrictor) has paved the way for development of prototype ACE inhibitor Eg: Captopril.
Renin is the limiting factor for Angiotensin II generation. Plasma half life of renin is 15 minutes. Biological potency of Angiotensin I is very short, hence it is rapidly converted into Angiotensin II by ACE a dipeptidyl carboxypeptidase located primarily on the luminal surface of vascular endothelial cells in lungs.
Angiotensin II has a very short half life (less than a minute). Angiotensin III is less potent and stimulate aldosterone secretion and Angiotensin III is acted on by angiotensinases to inactive metabolites.
Blood vessels contain circulating renin, angiotensinases and produce Angiotensin II within their wall. Locally renin-angiotensin system present in heart, blood vessels, brain, kidneys, adrenals generate Angiotensin II and operate locally.
Angiotensins receptors
Angiotensin receptors (AT) are present on the surface of target cells. two subtype receptors AT1 and AT2 have been identified. Losartan is the specific antagonist for AT1 receptor. All the effects of Angiotensin II are mediated through AT1 receptors.
AT2 receptors have been identified in adrenal medulla and CNS. AT1 receptor is a G-protein coupled receptor utilizing different transducer mechanism in different tissues. Phospholipase C – IP3/DAG and intracellular calcium ions release underlies vascular and visceral smooth muscle contraction by activating myosin light chain kinase. Membrane calcium ions are also activated.
Calcium movement induces aldosterone synthesis release, cardiac inotropy,depolarization of autonomic ganglia, adrenal medulla resulting catecholamine release and sympathetic outflow.
DAG activates protein kinase C which phosphorylase intracellular proteins and promotes cell growth. In liver and kidney Angiotensin II inhibits adenyl cyclase. Intrarenal homeostatic mechanism involves prostaglandin and leukotrienes production through activation of phospholipase A2.
This molecular mechanism has a wide effect on myocardium, vascular smooth muscle, fibroblasts through AT1 receptor where Angiotensin II has sustained effect on cell growth and intracellular matrix synthesis.
Pharmacological actions of angiotensin
CVS
- Prominent action is vasoconstriction through adrenaline or nor adrenaline or by increasing sympathetic outflow.
- Vasoconstriction is involved in all vascular beds with less marked constriction effects on cerebral, skeletal muscle, pulmonary and coronary vessels.
- It is more potent than nor adrenaline which promotes fluid movement from vascular to extravsacular compartment and cause rise of blood pressure
- Continuous perfusion cause a sustained rise of blood pressure and reabsorption of salt and water.
- Promote calcium ion influx and increase myocardial contraction.
- Increases heart rate by enhancing sympathetic outflow, cardiac output is reduced and cardiac work is increased.
- Contributes to the hypertrophy and remodelling of heart and blood vessels. ACE inhibitor retards/reverses many of these changes imparted by AII.
Smooth muscles
On many visceral smooth muscles invivo actions are insignificant.
Adrenal cortex
Angiotensin II and III are trophic in action enhances synthesis and release of aldosterone. Acts on distal tubules, promotes reabsorption of sodium ions and excretion of potassium and hydrogen excretion
Kidney
- Exerts indirect effect through aldosterone.
- Promotes sodium and potassium ion exchange in proximal tubule leading to increased sodium, chloride and bicarbonate ion reabsorption.
- Reduces renal blood flow resulting in sodium and water retention and increases potassium excretion.
CNS
- On systemic administration enter periventricular areas of the brain and induce drinking behavior and anti diuretic hormone release.
- Increases sympathetic outflow and contributes to pressor effects.
- Peripheral sympathetic structures act in response to adrenaline release from adrenal medulla and stimulation of autonomic ganglia.
Pathophysiological role of angiotensin II
Mineralocorticoid secretion
Angiotensin II is the stimulus for aldosterone secretion from adrenal cortex thereby persistently raise Angiotensin II levels.
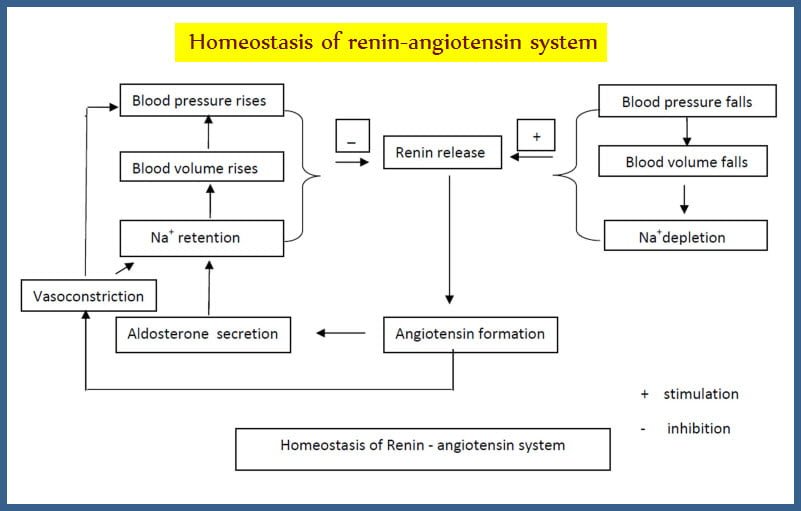
Electrolyte and pressure homeostasis
- Renin – angiotensin system sense decrease tension in the afferent glomerulosa arterioles through intrarenal baroceptor pathway and production of prostaglandins locally.
- Low concentration of sodium ions sensed by macula densa pathway
- Sympathetic outflow response by baroceptor to juxta glomerulus cells is sensed through beta adrenoreceptor pathway.
- In this situation increased renin is translated to angiotensin II causes an acute rise in blood pressure by vasoconstriction and long lasting rise in blood pressure by increasing sodium and water reabsorption in the kidney.
- Angiotensin II formed within kidney exerts local regulatory effects.
- The major pharmacological implications in the mechanism of release of renin are:
- ACE inhibitors and AT1 antagonists enhance renin release by interfering through feed back mechanism.
- Vasodilators and diuretics stimulate renin release by lowering blood pressure.
- Reduction of sodium ions into macula densa by loop diuretics cause renin release.
- Central sympatholytics and beta blockers decrease renin release.
- NSAIDs inhibit prostaglandin synthesis which in turn decrease renin release.
Develop secondary hyper aldosteronism due to renin angiotensin activation
CNS – Angiotensin II is formed locally and act as neurotransmitter or neuromodulator by which regulation of thirst, hormone release and sympathetic outflow is mediated.
Inhibition of Renin – Angiotensin System
Inhibition of Renin Angiotensin system can be achieved by-
- Sympathetic blockers which decrease renin release
- Renin inhibitory peptides and renin specific antibodies which interfere with generation of Angiotensin I from angiotensinogen
- ACE inhibitors like captopril prevent generation of Angiotensin II
- AT1 antagonist like losarton block action of Angiotensin II on target cells.
- Aldosterone antagonists like spironolactone blocks the mineralocorticoid receptors.
ACE inhibitors
ACE (Angiotensin converting enzyme) inhibitors are teprotide, captopril, enalapril, Lisinopril, Perindopril, Rampiril.
Teprotide – synthesized from bradykinin potentiating factor found in pit viper venom was the first ACE inhibitor which is a nanopeptide with brief duration of action.
Captopril– Orally active dipeptide analogue is a prototype of ACE inhibitor, Abolishes pressor action of Angiotensin I but not Angiotensin II, Increase plasma kinin levels and potentiate the hypotensive action of bradykinin, Elevated kinins and prostaglandins may be responsible for cough induced by ACE inhibitors.
Interferes with degradation of substance P, The lowering of blood pressure depends on sodium ion status and renin angiotensin activity, The hypotension is due to decrease of total peripheral resistance.
Both systolic and diastolic blood pressure falls. Renal, cerebral and coronary blood flow is not compromised, 70% of orally administered drug is absorbed, Food reduces the bioavailability, Partly metabolized and excreted unchanged in urine, Poorly crosses blood brain barrier.
Adverse Effects of Captopril
Captopril is a usually well tolerated drug. Occasionally hypotension,hyperkalaemia,cough,allergy,angiodema,dysguesia,foetal abnormalities, nausea, bowel upset, granulocytopenia,proteinuria, acute renal failure may occur.
Drug interactions in Captopril
NSAIDs attenuate hypotensive action and Antacids reduce bioavailability
Enalapril– Prodrug converted to enalaprilat – tripeptide analogue, Poorly absorbed.
Advantages of Enalapril
Enalapril is a more potent drug than captopril. Food does not affect absorption of enalapril and it have onset of action is slower but longer duration of action can be seen. Adverse effects is minimal.
Lisinopril
Lysine derivative of enalaprilat, Absorbed orally slowly, Food does not interfere with its absorption, Duration of action is longer permitting single daily dosing, Uniform hypotensive action, Minimal side effects with reduction in venous return, cardiac contractility and cardiac output.
Perindopril– Long acting ACE inhibitor, Slow onset of action, Undergoes extensive metabolism, Tends to restore the reduced elastic properties of arteries and heart in hypertensive.
Ramipril– Long acting ACE inhibitor, Extensive tissue distribution.
Clinical uses of angiotensin
Hypertension– Used as first line of drugs in all grades of hypertension.
Advantages of using angiotensins in Hypertension
No postural hypotension, electrolyte disturbances, weakness, and CNS effects, Safe for diabetic, asthmatics, peripheral vascular disease patients, Prevent secondary hyperaldosteronism and potassium loss due to diuretics, Renal flow is maintained, Reverse left ventricular hypertrophy, No adverse effect on lipid profile, No rebound hypertension on withdrawal, Increase the life expectancy of hypertensives.
Congestive Heart failure– Retard the progression of ventricular systolic dysfunction and prolong survival of CHF patients
Myocardial infarction– Advocated within 24 hours of attack and continued for more weeks – reduce early as well as long term mortality, irrespective of systolic dysfunction and hypotension is avoided.
Diabetic nephropathy– Prolonged therapy prevents end stage renal disease in both insulin and non insulin dependant situations. It is of value in diabetic nephropathy whether hypertensive or not.
Angiotensin antagonist
Angiotensins antagonist are Saralasin and Losartan
Saralasin
- An octapeptide analogue of Angiotensin II
- Exhibited partial agonistic activity
- Need parenteral administration only.
Losartan
- Competitive antagonist
- Devoid of partial agonistic activity
- Selective antagonist of AT1 receptor
- Blocks all actions of Angiotensin II namely vasoconstriction, central and peripheral sympathetic outflow action, aldosterone release, salt and water reabsorption, growth promoting actions on heart and blood vessels.